PROMPT Precision Health Study surpasses 1,000 participants

Recruiting since May 2020, the study on mobile technology in mental health care tracks both passive and patient-reported data to learn how to get the most effective individual treatment to patients as quickly as possible.
Since Precision Health at U-M’s inception, mental health care was identified as a priority area that could benefit from a precision-health approach. With the PROviding Mental health Precision Treatment (PROMPT) Precision Health Study, “We want to address two fundamental problems,” said PROMPT Co-Investigator Amy Bohnert, PhD, Professor of Anesthesiology, Psychiatry, and Epidemiology: “In mental health care, there’s a huge problem with long waits for care.” She and Co-Investigator Srijan Sen, MD, PhD, Director of the Frances and Kenneth Eisenberg and Family Depression Center, designed PROMPT so that participants’ needs are addressed not when they reach the clinic, but as early as possible, by offering mobile treatments.
The second problem the project seeks to address is the “one size fits all” approach that has been the standard for mental health treatment, with patients often cycling through multiple rounds of treatments until they find one that works. “We hope to more effectively bring a precision approach to mental health and be able to predict beforehand which treatment will be most effective for a specific patient,” said Sen.
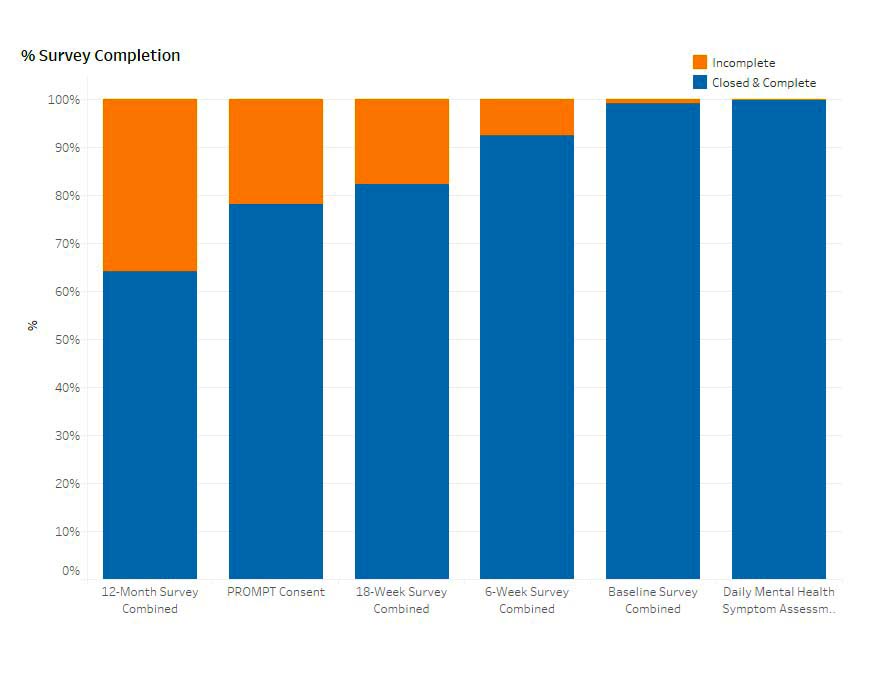
The study was designed to collect a rich array of biologic, behavioral, social, and symptom data from participants. Collection methods include Fitbits, a “spit kit” (a DNA saliva collection kit with a pre-paid return envelope), daily mood ratings via the MyDataHelps app, and 20-minute surveys at six weeks, 18 weeks, and one year after enrollment. To date, 92% of enrolled patients submitted six-week follow up surveys, and 81% completed 18-week surveys. The average completion rate of daily mood score surveys during the first six weeks has been 82.6%—a high level of engagement for a daily study.
Incorporating genetic samples and objective sleep and activity measurements are part of PROMPT’s “goal to capture domains critical to mental health that will improve our capacity to accurately match patients to the treatment that will work for them,” Sen said. In addition, these measures have the potential to serve as early signs of treatment response. “Ideally, in the future we’ll be able to say, ‘this person is on a trajectory toward improving’ or ‘this person doesn’t show signs of responding to their current treatment,’ and have objective measures of change to guide treatment within a few weeks, rather than a few months,” Bohnert added.
As the study progresses, the investigators hope to tap into Precision Health’s Analytics Platform’s resources, such as geolocation and Surescripts information, to supplement the data they’re collecting.
The PROMPT study tracks participants’ in-clinic treatments and considers the role of mobile interventions as part of a broader therapy plan. “There’s suggestive evidence that mobile mental health treatments work, but mostly as short-term trials outside of existing care systems,” said Bohnert. “We want to test mobile interventions in a way that’s integrated into the flow of patient care under real-world conditions. We’re looking at what [mobile interventions] can add for patients who are also going to get therapy or also get medications, depending on what their clinical team decides.”
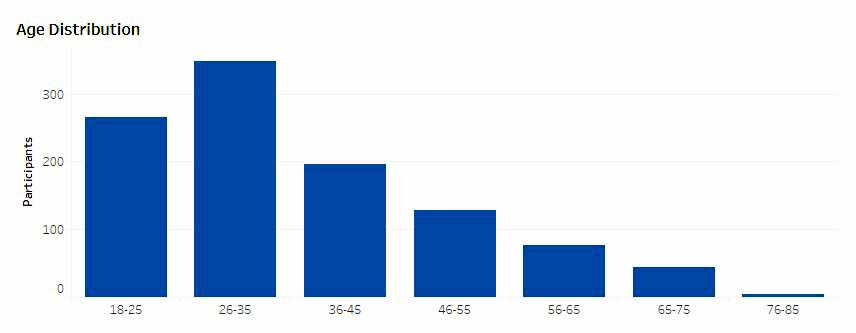
To date, more than 1,100 participants, 72% of them female (which is aligned with the gender distribution of those seeking mental health care, Bohnert said), have enrolled in PROMPT, ranging in age from 18 to 80.
 Sen and Bohnert are planning to expand their research into mental health treatments in primary care, and to develop and test a reinforcement learning algorithm to match patients to treatments. Among PROMPT participants to date, there has been substantial decreases in symptoms over six weeks of mobile intervention use, with different patterns of sleep, cardiac, and physical activity changes with different mobile treatment types.
Sen and Bohnert are planning to expand their research into mental health treatments in primary care, and to develop and test a reinforcement learning algorithm to match patients to treatments. Among PROMPT participants to date, there has been substantial decreases in symptoms over six weeks of mobile intervention use, with different patterns of sleep, cardiac, and physical activity changes with different mobile treatment types.
Through a collaboration with Precision Health’s Data Analytics & IT Workgroup, they are working to make PROMPT data accessible to secondary users across campus. “We’re looking for people who want to run with it and look in the data and publish what they find…we don’t see it as just our study,” said Bohnert.
The PROMPT study draws on the expertise of researchers and schools across campus, including Emily Mower Provost, PhD, and Jenna Wiens, PhD, from the College of Engineering; Daniel Forger, PhD, and Ambuj Tewari, PhD, from LSA; Corey Lester, PharmD, PhD, from the College of Pharmacy; and Walter Dempsey, PhD, and Zhenke Wu, PhD, from the School of Public Health. Partner organizations on the project include Michigan Medicine Outpatient Psychiatry (for recruitment of community members), and University Health Service (for recruitment of students).


